Catastrophic out of pocket medicine expenditure: A case for monitoring performance of primary providers on national health insurance scheme
https://doi.org/10.51412/psnnjp.2023.33
Keywords:
Essential medicines, Health insurance, Impoverishment, Out of stock, Stock outsAbstract
Background: One of the critical components of national health insurance scheme is the financial protection it provides to patients by reducing out of pocket (OOP) healthcare expenditure.Among low income patients even a little OOP payments due to medicine unavailability of medicines can be financially catastrophic for households. The lack of medicines is not a new phenomenon, however it was expected that funding from health insurance will improve availability and significantly reduce or eliminate OOP for medicines. The effect of OOP medicines payments on impoverishment among insured patients remain largely unexplored in the country. This study therefore aim to determine OOP medicine payments and its impoverishing effect on patients living on national minimum wage.
Methods: This was a retrospective study using prescription records at the national health insurance pharmacy unit of the University of Maiduguri teaching hospital. A total of 2036 were selected by simple random method and reviewed for evidence of medicine unavailability (January 2022 – December 2022). Medicines for which “not available” (N/A) and “out of stock” (O/S) were indicated was considered to be unavailable at the time of filling the prescription. The cost for one month supply of drugs for non-communicable diseases (NCDs) and ten day supply for other drug classes was computed using average private and public sector prices for analysis. The data was analyzed using descriptive statistics and national minimum wage of N30,000/month ($40) at the exchange rate of $1 = N750.
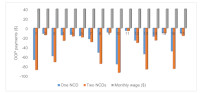
Results: The profile of unavailable medicines indicated that all class of drug were affected (47 – 100%). The estimated OOPpayments due to medicine stock out resulted in catastrophic expenditure of 12 – 232.5% of minimum wage and impoverishment rate of 12 – 132%. The protecting effect of health insurance was erased by the OOP payments leaving patients with impoverishment and inability to afford medicines.
Conclusion: There is need to regularly review of provider performance with respect to medicine availability, so as to protect the most vulnerable from catastrophic OOPmedicine expenditure.
References
World Health Organization WHO Health systems financing: the path to universal coverage. Geneva: World Health Organization; 2012 https://apps.who.int/iris/handle/10665/44371. Accessed th on 13 July 2023
United Nations. Sustainable development goals: 1 7 g o a l s t o t r a n s f o r m o u r w o r l d . 2 0 1 5 . http://www.un.org/sustainabledevelopment/. Accessed on 13th July 2023
Barasa EW, Maina T, Ravishankar N (2017) Assessing the impoverishing effects, and factors associated with the incidence of catastrophic health care payments in Kenya. International Journal for Equity in Health. 16:31 https://doi: 10.1186/s12939-017-0526-x
Adesina AD and Ogaji DS (2018) Impoverishing effect of household healthcare expenditure in semi-rural communities in Yenagoa, Nigeria. Healthcare in Lowr e s o u r c e S e t t i n g s 6 : 7 4 6 4 https://doi.org/10.4081/hls.2018.7464
World Health Organization's Report. Health system financing: the path to universal coverage. 2010. https://apps.who.int/iris/handle/10665/44371. Accessed th on 5 July 2023
Onoka CA, Onwujekwe OE, Uzochukwu BS, Ezumah NN (2013) Promoting universal financial protection: constraints and enabling factors in scaling- up coverage with social health insurance in Nigeria. Health Research and Policy System 11:20 https://doi.org/10.1186/1478-4505-11-20
World Bank, 2016. World Development Indicator (WDI) 2016 http://databank.worldbank.org Accessed on 12th July 2023
Hafez R (2018) Nigeria health financing system assessment. Discussion Paper, World Bank. https://doi.org/10.1596/30174
World Health Organization. Public financing for health in Africa: from Abuja to the SDGs. Geneva: World Health Organization; 2016. WHO/HIS/HGF/Tech.Report/16.2 Accessed on 10th July 2023
Sayuti M and Sukeri S (2022) Assessing progress towards sustainable development goal 3.8.2 and determinants of catastrophic health expenditures in Malaysia. Plos One 17(2): e0264422 https://doi.org/10.1371/journal.pone.0264422
Sum G, Hone T and Lee JT (2018) Multimorbidity and out-of-pocket expenditure on medicines: a systematic review. BMJ Global Health 3:e000505 https://doi: 10.1136/bmjgh-2017-000505
Kankeu HT, Saksena P, Xu K, Evans DB (2013) The financial burden from non-communicable diseases in low- and middle-income countries: a literature review. Health Research and Policy System 11: 31 https://doi: 10.1186/1478-4505-11-31
Wagstaff A, Flores G and Eozenou P (2018) Progress on catastrophic health spending in 133 countries: a retrospective observational study. The Lancet Global Health 6: e169–79 https://doi: 10.1016/S2214-109X(17)30429-1
Hailemichael Y, Hanlon C and Hailemariam D ( 2 0 1 9 ) C a t a s t r o p h i c h e a l t h e x p e n d i t u r e a n d impoverishment in households of persons with depression: a cross-sectional, comparative study in rural Ethiopia. BMC Public Health 19: 930 https://doi.org/10.1186/s12889-019- 7239-6
Jan S, Lee SW and Huo Y (2016) Catastrophic health expenditure on acute coronary events in Asia: a prospective study. Bulletin of the World Health Organization 94: 193 https://doi: 10.2471/BLT.15.158303
Okoronkwo IL, Ekpemiro JN, Okwor EU, Okpala PU, Adeyemo FO (2015) Economic burden and catastrophic cost among people living with type2 diabetes mellitus attending a tertiary health institution in south-east z o n e , N i g e r i a . B M C R e s e a rc h N o t e s 8 : 5 2 7 https://doi.org/10.1186/s13104-015-1489-x
Salari P, Di Giorgio L, Ilinca S, Chuma J (2019) The catastrophic and impoverishing effects of out-ofpocket healthcare payments in Kenya. BMJ Global Health 4:e001809 https://doi:10.1136/bmjgh-2019-001809
Jaspers L, Colpani V and Franco OH (2015) The global impact of non-communicable diseases on households and impoverishment: a systematic review. European Journal of Epidemiology 30:163–88 https://doi: 10.1007/s10654-014-9983-3
Lee JT, Hamid F and Millett C (2015) Impact of non-communicable disease multi-morbidity on healthcare utilization and out-of-pocket expenditures in middleincome countries: cross sectional analysis. Plos One 10:e0127199 https://doi: 10.1371/journal.pone.0127199
Jan S, Laba T-L and Atun R (2018) The Lancet Taskforce on NCDs and economics 3 Action to address the household economic burden of non- communicable diseases. Lancet 391: 2047–2058 https://doi: 10.1016/S0140-6736(18)30323-4
Kiil A and Houlberg K (2014) How does copayment for health care services affect demand, health and redistribution? A systematic review of the empirical evidence from 1990 to 2011. European Journal of Health Economics HEPAC 15: 813 https://doi: 10.1007/s10198- 013-0526-8
Negin J, Randell M and Kowal P (2016) Health expenditure and catastrophic spending among older adults living with HIV. Global Public Health 12: 1–15 https://doi: 10.1080/17441692.2016.1173717
Azzani M, Roslani AC, Su TT (2015) The perceived cancer-related financial hardship among patients and their families: A systematic review. Support Care Cancer 23: 889–898 https://doi: 10.1007/s00520-014-2474-y
Xin XX, Guan XD, Shi LW (2016) Catastrophic expenditure and impoverishment of patients affected by 7 rare diseases in China. Orphanet Journal of Rare Diseases 11: 74 https://doi.org/10.1186/s13023-016-0454-7
van Doorslaer E, O'Donnell O and Zhao Y (2007) Catastrophic payments for health care in Asia. Health Economics 16: 1159–1184 https://doi:10.1002/hec.1209
Hadley J (2007) Insurance coverage, medical care use, and short-term health changes following an unintentional injury or the onset of a chronic condition. Journal of American Medical Association 297: 1073–1084 https://doi:10.1001/jama.297.10.1073
Fatima SA and Khaliq A (2017). A survey regarding drug shortage in tertiary care hospitals of Karachi, Pakistan. Journal of Pharmacy Practice and C o m m u n i t y M e d i c i n e 3 ( 4 ) : 2 6 2 – 2 6 6 http://dx.doi.org/10.5530/jppcm.2017.4.69
Martei YM, Grover S and DeMichele A (2019). Impact of essential medicine stock outs on cancer therapy delivery in a resource-limited setting. Journal of Global Oncology 5: 1 –11 https://doi: 10.1200/JGO.18.00230
Mukundiyukuri JP, Irakiza JJ and Hedt-Gauthier B (2020) Availability, costs and stock-outs of essential NCD drugs in three rural Rwandan districts. Annals of Global Health. 86(1): 123 https://doi: 10.5334/aogh.2729
Hordes R, Price I and Cluver L (2017) How frontline healthcare workers respond to stock-outs of essential medicines in the Eastern Cape province of South Africa. South African Medical Journal 107(9): 738-740 https://doi: 10.7196/SAMJ.2017.v107i9.12476
Ndzamela S and Burton S (2020) Patients and healthcare professionals' experiences of medicine stockouts and shortages at a community healthcare centre in the Eastern Cape. South African Pharmaceutical Journal 87(5): 37i-37m
Wagenaar BH, Gimbel S and Sherr K (2014) Stock-outs of essential health products in Mozambique - longitudinal analyses from 2011 to 2013. ropical Medicine and International Health 19(7):791–801
Osuafor NG, Ukwe CV, Okonta M (2021) Evaluation of availability, price, and affordability of cardiovascular, diabetes, and global medicines in Abuja, Nigeria. Plos One 16(8): e0255567 https://doi: 10.1111/tmi.12314 Ozoh
OB, Eze JN and Beran D (2021) Nationwide survey of the availability and affordability of asthma and COPD medicines in Nigeria. Tropical Medicine and International Health 26(1): 54 -65 https://doi:10.1111/tmi.13497
Hawley KL, Mazer-Amirshahi M and Pines JM (2016) Longitudinal trends in U.S. shortages for medications used in emergency departments [2001 – 2014]. Academic Journal of Emerging Medicine 23(1): 63 – 69 https://doi: 10.1111/acem.12838
Pulcini C, Beovic B and Sharland M (2017) Ensuring universal access to old antibiotics: a critical but neglected priority. Clinical Microbiology and Infection 23(9): 590–592 https://doi: 10.1016/j.cmi.2017.04.026
Nurse-Findlay S, Taylor MM and Pyne-Mercier L (2017) Shortages of Benzathine Penicillin for prevention of mother-to-child transmission of syphilis: An evaluation from multi-country surveys and stakeholder interviews. Plos Medicine 14(12): e1002473 https://doi: 10.1371/journal.pmed.1002473 Sun
J, Hu CJ and Liu Y (2018) A review of promoting access to medicines in China - problems and recommendations. BMC Health Services Research 18: 125 https://doi.org/10.1186/s12913-018-2875-6
Gong S, Cai H and Jin S (2018) The availability, price and affordability of antidiabetic drugs in Hubei province, China. Health Policy Planning 33: 937– 947 https://doi.org/10.1093/heapol/czy076
Nchakoa E, Bussella S, Nesbetha C, Odoh C (2018) Barriers to the availability and accessibility of controlled medicines for chronic pain in Africa. International Health 10(2): 71–77. https://doi: 10.1093/inthealth/ihy002
Knaul FM, Farmer PE and Rajagopa MR (2018) Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the Lancet Commission report. Lancet 391(10128): 1391 – 1454 https://doi: 10.1016/S0140-6736(17)32513-8
Ashigbie PG, Rockers PC, Laing RO, Cabral HJ, Onyango MA, Likalamu JP, Wirtz VJ (2020) Availability and prices of medicines for non-communicable diseases at health facilities and retail drug outlets in Kenya: a crosssectional survey in eight counties. BMJ Open 10:e035132 http://dx.doi.org/10.1136/bmjopen-2019-035132
Acosta A, Vanegas EP, Rovira J, Godman B and Bochenek T (2019) Medicine shortages: Gaps between countries and global perspectives. Frontiers Pharmacology 10: 763 https://doi.org/10.3389/fphar.2019.00763
Al-Hanawi MK, Mwale ML and Qattan AMN (2021) Health insurance and out-of-pocket expenditure on health and medicine: heterogeneities along income. F r o n t i e r s P h a r m a c o l o g y 2 : 6 3 8 0 3 5 https://doi.org/10.3389/fphar.2021.638035
Tirgil A, Dickens WT, Atun R (2019) Effects of expanding a non-contributory health insurance scheme on out-of-pocket healthcare spending by the poor in Turkey. B M J G l o b a l H e a l t h 4 : e 0 0 1 5 4 0 . http://dx.doi.org/10.1136/bmjgh-2019-001540
Wirtz VJ, Servan-Mori E and Laing R (2022) Probability and amount of medicines expenditure according to health insurance status in Kenya: A household survey in eight counties. International Journal of Health P l a n n i n g a n d M a n a g e m e n t 3 7 ( 2 ) : 7 2 5 – 7 3 3 https://doi.org/10.1002/hpm.3368
Acharya A, Vellakkal S and Ebrahim S Impact of national health insurance for the poor and the informal sector in low- and middle-income countries: a systematic review. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2012 http://eppi.ioe.ac.uk/cms/Default.aspx?tabid=3346 Accessed 14th July 2023
Deutsche Gesellschaft fuÈ r Internationale Zusammenarbeit (GIZ) GmbH. (2015) Health Insurance for India's poor: Meeting the challenge with information technology. A publication in the German Health Practice Collection 2015 w w w . h e a l t h . b m z . d e / g o o d - practices/GHPC/Health_Insurance_India_New/RSBY_E N_long-Oct-2011.pdf Accessed 9th July 2023
Ghosh S (2014) Equity in the utilization of healthcare services in India: evidence from national sample survey. International Journal of Health Policy Management 2(1): 29 - 38 https://doi: 10.15171/ijhpm.2014.06
Jain N, Kumar A, Nandraj S, Furtado KM (2015) NSSO 71st round same data, multiple interpretations. Economic and Political Weekly 50 (46 & 47): 84 - 87 https://www.jstor.org/stable/44002870
S u n d a r a r a m a n T, M u r a l e e d h a r a n V R , Mukhopadhyay I (2016) NSSO 71st round data on health and beyond questioning frameworks of analysis. Economic and Political Weekly 51 (3): 85 – 88 https://www.jstor.org/stable/44004209
Aregbeshola BS and Khan SM (2018) Out-ofpocket payments, catastrophic health expenditure and poverty among households in Nigeria 2010. International Journal of Health Policy Management 7(9): 798–806 https://doi: 10.15171/ijhpm.2018.19
Edeh HC (2022) Exploring dynamics incatastrophic health care expenditure in Nigeria. Health Economics Review 12: 22 https://doi.org/10.1186/s13561- 022-00366-y
Beogo I, Huang N, Gagnon MP, Amendah DD (2016) Out of pocket expenditure and its determinants in the context of private healthcare sector expansion in sub - Saharan Africa urban cities: evidence from household survey in Ouagadougou, Burkina Faso. BMC Research Notes 9: 1–10 https://doi.org/10.1186/s13104-016-1846-4
Cherny NI, Sullivan R and Eniu A (2017) ESMO International consortium study on the availability, out-ofpocket costs and accessibility of antineoplastic medicines in countries outside of Europe. Annals of Oncology 28(11):2633–2647 https://doi: 10.1093/annonc/mdx521
Mekuria GA and Ali EE (2023) The financial burden of out of pocket payments on medicines among households in Ethiopia: analysis of trends and contributing f a c t o r s . B M C P u b l i c H e a l t h 2 3 : 8 0 8 https://doi.org/10.1186/s12889-023-15751-3
Selvaraj S, Farooqui HH, Karan A (2018) Quantifying the financial burden of households' out-ofpocket payments on medicines in India: a repeated crosssectional analysis of national sample survey data, 1994–2014. BMJ Open 8(5): 1–10 https://doi: 10.1136/bmjopen-2017-018020
Kuwawenaruwa A, Wyss K and Tediosi F (2020) The effects of medicines availability and stock-outs on household's utilization of healthcare services in Dodoma region, Tanzania. Health Policy Planning 35(5): 323–333 https://doi: 10.1093/heapol/czz173
Gabrani J, Schindler C, Wyss K (2022) Out of pocket payments and access to NCD medication in two regions in Albania. Plos One 17(8): e0272221 https://doi.org/10.1371/journal.pone.0272221
WHO (2018) New perspectives on global health spending for universal health coverage. World Health O r g a n i z a t i o n http://www.who.int/health_financing/topics/resourcetracking/new-perspectives/en/.Accessed 8th July 2023
Prinja S, Bahuguna P, Tripathy JP, Kumar R (2015) Availability of medicines in public sector health facilities of two North Indian States. BMC Pharmacology and Toxicology 16: 43 https://doi: 10.1186/s40360-015-0043-8
Bigdeli M, Laing R, Tomson G, Babar ZU (2015) Medicines and universal health coverage: challenges and opportunities. Journal of Pharmaceutical Policy and Practice 8: 8 https://doi.org/10.1186/s40545-015-0028-4
Dorjdagva J, Batbaatar E and Kauhanen J (2016) Catastrophic health expenditure and impoverishment in Mongolia. International Journal of Equity in Health. 15(1):105 https://doi.org/10.1186/s12939-016-0395-8
Ichoku HE, Fonta WM, Onwujekwe O (2009) Incidence and intensity of catastrophic health care financing and impoverishment due to out-of-pocket payments in southeast Nigeria. Journal of Insurance and Risk Management 4(4): 47-59
Wang H, Torres LV, Travis P (2018) Financial protection analysis in eight countries in the WHO SouthEast Asia Region. Bulletin of World Health Organization 96(9): 610–620E https://doi: 10.2471/BLT.18.209858
McHenga M, Chirwa GC, Chiwaula LS (2017) Impoverishing effects of catastrophic health expenditures in Malawi. International Journal of Equity in Health 16: 25 https://doi.org/10.1186/s12939-017-0515-0
Views | PDF Downloads:
568
/ 251
/ 0
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Nigerian Journal of Pharmacy

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.


