Prescribing Pattern and Errors in the Prescriptions for Outpatients with Diabetes Mellitus at a Nigerian University Health Centre
DOI:
https://doi.org/10.51412/psnnjp.2024.19Keywords:
diabetes mellitus, prescribing errors, prescribing patterns, anti-diabetic medicationsAbstract
Background: Findings have revealed that prescribing errors are increasingly common in diabetes mellitus drug therapy mainly because of polypharmacy. An important way to tackle this problem is through regular prescription auditing.
Objectives: This study aimed to assess the prescribing pattern of prescriptions received from outpatients with diabetes mellitus at a Nigerian University Health Centre and identify prescribing errors in the prescriptions.
Methods: Across-sectional study of prescriptions from outpatients who visited the Main Pharmacy of Obafemi Awolowo University Health Centre between January 28, 2020, and March 18, 2020, was conducted. The study included prescriptions for patients covered by the National Health Insurance Agency (NHIA) and contained orders for at least one medication for diabetes mellitus. Drug information and patient demographics were assessed for prescribing patterns and errors. Descriptive statistical analysis of the data was carried out using Microsoft Excel 2010.
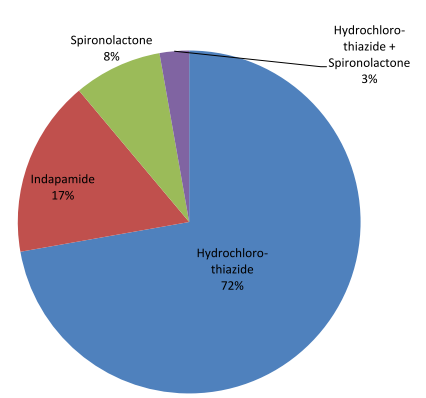
Results: Atotal of 261 prescriptions containing at least one anti-diabetic medication were studied. All the patients were described as 'adults' but the exact ages were not indicated on the prescriptions. The medications were mostly prescribed in their brand names and metformin was the most prescribed drug either alone or in combination with other antidiabetic agents. A small percentage (4.2%) of the prescriptions had prescribing errors, a total of 11 in them. These errors included medication strength omissions, incorrect dosage, and therapy duration omissions.
Conclusions: We identified 11 prescribing errors from the outpatient prescriptions used in this study. Most times, these errors were identified by the clinical pharmacists on duty and were resolved either by communicating with the prescribers or using their professional discretion.
References
Araújo F, Fonte P, Santos HA, Sarmento B (2012) Oral delivery of glucagon-like peptide-1 and analogs: alternatives for diabetes control? Journal of Diabetes Science and Technology 6(6):1486-97. DOI: 10.1177/193229681200600630.
International Diabetes Federation. IDF Diabetes th Atlas. 9 ed. Brussels, Belgium, 2019. https://www.diabetesatlas.org. Accessed January 31, 2021.
Cox AR, Ferner RE (2009) Prescribing errors in diabetes. The British Journal of Diabetes & Vascular Disease 2: 84 - 8. DOI: 10.1177/1474651409103902.
Shrestha R, Prajapati S (2019) Assessment of prescription pattern and prescription error in outpatient Department at Tertiary Care District Hospital, Central Nepal. Journal of Pharmaceutical Policy and Practice 12:1-9. DOI: 10.1186/s40545-019-0177-y.
Shareef JA, Fernandes JE, Samaga LA, Khader SA (2016) A study on adverse drug reactions in hospitalized patients with diabetes mellitus in a multi-speciality teaching hospital. Asian Journal of Pharmaceutical Clinical Research 9(2):114-7.
Demoz GT, Berha AB, Alebachew Woldu M, Yifter H, Shibeshi W, Engidawork E (2019) Drug therapy problems, medication adherence and treatment satisfaction among diabetic patients on follow-up care at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. PloS one 14 (10): e 0222985. DOI: 10.1371/journal.pone.0222985.
Stepka M, Rogala H, Czyzyk A (1993) Hypoglycemia: a major problem in the management of diabetes in the elderly. Aging (Milano)5 (2): 117 - 21. DOI: 10.1007/BF03324137. PMID: 8323998.
Arul B, Jitty SM, Lekshimi M, Krishna PTK, Kothai R (2018) Prescription analysis of statins in patients with cardiovascular diseases and other comorbidities in various tertiary care hospitals at Salem district, Tamil Nadu. International Journal of Research in Pharmaceutical Sciences 10(1): 668-672. DOI: 10.26452/ijrps.v10i1.1899.
Breuker C, Abraham O, Di Trapanie L, Mura T, Macioce V, Boegner C, Jalabert A, Villiet M, Castet-Nicolas A, Avignon A, Sultan A (2017) Patients with diabetes are at high risk of serious medication errors at hospital: Interest of clinical pharmacist intervention to improve healthcare. European Journal of Internal Medicine 38:38-45. DOI: 10.1016/j.ejim.2016.12.003.
Diabetes Association of Nigeria (2013) Clinical Practice Guidelines for Diabetes Management in nd Nigeria. 2 ed. Bendik Printing Press : PortHarcourt, Nigeria, pp1-77.
Mahmood M, Reddy RC, Lahari JS, Fatima S, Shinde P, Reddy SA (2017) Prescription pattern analysis of antidiabetic drugs in diabetes mellitus and associated comorbidities. Clinical Investigation (Lond.) 8(1):5-12. DOI: 10.4172/Clinical-Investigation.1000123.
Elliott WJ (2012) Effects of potassium-sparing versus thiazide diuretics on glucose tolerance: new data on an old topic. Hypertension 59(5):911-2.DOI:10.1161/HYPERTENSIONAHA.112.192542.
Scheen AJ (2018) Type 2 diabetes and thiazide diuretics. Current diabetes reports 18:1-3.
Razmaria AA (2016) Generic drugs. Jama 315(24):2746. DOI:10.1001/jama.2016.3990.
Downloads
Views | PDF Downloads:
409
/ 183
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 The Nigerian Journal of Pharmacy

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.


