Assessment of knowledge and counselling on ophthalmic preparations among community pharmacists in Ibadan, Nigeria – an intervention study
https://doi.org/10.51412/psnnjp.2022.22
Keywords:
Counselling, Intervention Study, Knowledge, Ophthalmic Preparations, PharmacistsAbstract
Background: The ratio of patients to ophthalmologists is rather high, affffording inadequate time for patient interaction, especially on the use of ophthalmic preparations. An assessment of community pharmacists' knowledge and counselling on ophthalmic preparations is vital to maintaining quality of care received by patients.
Methods: A cross-sectional study was carried out among consented community pharmacists practicing in Ibadan metropolis in southwest Nigeria, who were randomized into control and intervention arms. Baseline assessment of their knowledge and counselling on ophthalmic preparations was done. An educational intervention was then carried out among the intervention pharmacists. Postintervention assessment was carried out to evaluate the effffect of the intervention. Data was summarized with descriptive and inferential statistics.
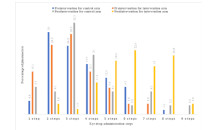
Results: A total of 115 (control arm-62; intervention arm-53) community pharmacists participated in the study. Percentage of community pharmacists who understood punctal occlusion (control vs intervention) increased from 21.0% vs 22.6% at baseline to 45.4% vs 83.0% postintervention. Preintervention (control vs intervention), 83.9% vs 81.1% knew that eye drop bottle tip should not touch the eyes during application. This improved postintervention to 82.3% vs 100%. A signifificant difffference in participants' knowledge and counselling on ophthalmic preparations was observed postintervention. Participants' knowledge comparison (control vs intervention) was 7.79 ± 1.79 vs 7.60 ± 1.65 (p = 0.565) and 8.89 ± 1.73 vs 10.83 ± 1.63 (p < 0.001) at baseline and postintervention, respectively. The counselling comparison (control vs intervention) was 2.82 ± 1.93 vs 2.57 ± 1.91 (p = 0.476) at baseline, and 2.97 ± 2.48 vs 5.98 ± 1.69 (p < 0.001) postintervention.
Conclusion: The educational intervention, which addressed the knowledge and counselling gaps discovered at baseline, improved the community pharmacists' knowledge and counselling on ophthalmic preparations.
References
Gupta R, Patil B, Shah B. M, Bali SJ, Mishra SK and Dada, T. (2012). Evaluating eye drop instillation technique in glaucoma patients. Journal of Glaucoma 21(3): 189–192 doi: 10.1097/ijg.0b013e31820bd2e1
Tatham AJ, Sarodia U, Gatrad F and Awan A (2013). Eye drop instillation technique in patients with glaucoma. The bioadhesion goal. International Journal of Pharmacy 531: 167–178 doi: 10.1038/eye.2013.187
Carpenter DM, Sayner R, Blalock SJ, Muir KW, Hartnett ME, Lawrence SD, Giangiacomo AL, Goldsmith JA, Tudor GE, Robin AL and Sleath BL. (2016). The effect of eye drop technique education in patients with glaucoma. Health Community 31(8): 1036 – 1042 doi: 10.1080/10410236.2015.1020263.
Schwartz GF, Hollander DA and Williams JM. (2013). Evaluation of eye drop administration technique in patients with glaucoma or ocular hypertension. Current Medical Research Opinion 29(11): 1515 – 1522 doi:10.1185/03007995.2013.833898.
Davis SA, Sleath B, Carpenter DM, Blalock SJ, Muir KW and Budenz DL. (2018). Drop instillation and glaucoma. Current opinion in ophthalmology 29(2): 171 – 177 doi: 10.1097/ICU.0000000000000451.
Megbelayin OE, Babalola OY, Opubiri Y, Adenuga O, Akinyemi A and Megbelayin F. (2013). KAPs of pharmacists attending to
ophthalmic patients in Nigerian public hospitals. Journal of Pharmacy and Biological Sciences 7(6): 5-8.
Weekes L and Ramzan I. (2020). Prescription of compounded ophthalmic medications: a pharmacy perspective. Clinical and Experimental Optometry doi:10.1111/cxo.13066.
McVeigh KA and Vakros G. (2015). The eye drop chart: a pilot study for improving administration of and compliance with topical treatments in glaucoma patients. Clinical ophthalmology (Auckland, N. Z.) 9: 813 – 819 doi: 10.2147/OPTH.S82909.
Lampert A, Bruckner T, Haefeli WE and Seidling HM. (2019). Improving eye-drop administration skills of patients - A multicenter parallel-group cluster-randomized controlled trial. PloS one 14(2), e0212007. https://doi.org/10.1371/journal.pone.0212007.
Oyebode AA and Aje AA. (2022). Intervention study on pharmacists' knowledge and counseling on ophthalmic preparations in a tertiary hospital in south-western Nigeria. Malaysian Journal of Pharmaceutical Sciences 20 (1): 73–84 doi.org/10.21315/mjps2022.20.1.6
Mehuys E, Delaey C, Christiaens T, Van Bortel L, Van Tongelen I, Remon J. P and Boussery K. (2020). Eye drop technique and patient-reported problems in a real-world population of eye drop users. Eye (London, England) 34(8): 1392–1398
doi: 10.1038/s41433-019-0665-y.
Arunkumar S, Banagar B and Chanda. (2014). Eye drop instillation, a skill to be taught? Journal of Educational Research & Medical Teacher 2(2): 20-22.
Views | PDF Downloads:
920
/ 309
/ 0
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.


