Effect of Nevirapine-based Antiretroviral Therapy on the Treatment Outcome of Uncomplicated Malaria with Artemether-Lumefantrine among HIV-infected children
Keywords:
Drug-drug interaction, Artemether-lumefantrine, Malaria treatment outcome, HIV/AIDS, ChildrenAbstract
Background: The geographical overlap of malaria and HIV in sub-Saharan Africa posed a major public health challenge, which is further worsened by the potential interactions between antimalarial and antiretroviral drugs when co-administered. This study aimed to compare the responses to artemether/lumefantrine (AL) treatment among HIV-infected children on nevirapine based highly active antiretroviral therapy (HAART) and HIV-non-infected children that were positive for Plasmodium falciparummalaria parasites.
Methods: This is a multi-centered, prospective, non-randomized, open-labelled study with two arms consisting of HIV- infected children on nevirapine-based HAART (NVP-arm; n=32) and HIV-non infected children (control-arm; n=40). Both groups of patients were treated with ALafter microscopic confirmation of P. falciparum and were actively monitored for 28 days for efficacy and safety. Primary outcome was Adequate Clinical and Parasitological Response (ACPR) after treatment with ALby day
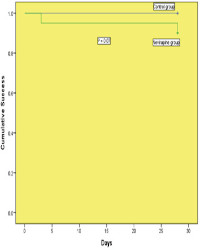
Results: Day 28 ACPR was lower in the NVP-arm (90%) compared to the control-arm (100%) of the study. In the NVP- arm of the study, 5% of cases had early treatment failure and 5% had late parasitological failure. The cumulative risk of developing recurrent malaria in NVP-arm was not statistically significantly higher than in the control-arm (P= 0.07). The reported potential adverse reactions to ALwere mild and included cough, pyrexia, anorexia, and abdominal pain. The cumulative risk of developing cough, pyrexia, anorexia and abdominal pain between NVP-arm compared to the control-arm was not statistically significant (Hazard ratio [HR], 0.51, 0.79 and 0.37 [95% confifidence interval {CI}, 0.04–5.26, 0.07-9.32, and 0.04- 3.56]; P= 1.000, 1.000, and 0.637) respectively.
Conclusion: Treatment of uncomplicated malaria with AL was safe and effffective after 28 days of follow-up in HIV- infected children on NVP. Nevirapine based HAARTmay, however, lead to delayed parasite clearance in children treated with AL.
References
WHO (2020) World malaria report 2020: 20 years of global progress and challenges. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO https://www.who.int/publications/i/item/9789240015791. Accessed September 20, 2021
Ashley EA, Stepniewska K, Lindegårdh N, McGready R, Annerberg A, Hutagalung R, Singtoroj T, Hla G, Brockman A, Proux S, Wilahphaingern J, Singhasivanon P, White NJ, Nosten F. (2007) Pharmacokinetic study of artemether- lumefantrine given once daily for the treatment of uncomplicated multidrug-resistant falciparum malaria. Tropical Medicine and International Health 12: 201–8. DOI:10.1111/j.1365-3156.2006.01785.x
Tarning J, Kloprogge F, Dhorda M, Jullien V, Nosten F, White NJ, Guerin PJ, Piola P. (2013) Pharmacokinetic properties of artemether, dihydroartemisinin, lumefantrine, and quinine in pregnant women with uncomplicated Plasmodium falciparum malaria in Uganda. Antimicrobial AgentS Chemotherapy 57: 5096 – 103. DOI: 10.1128/AAC.00683-13
White N.J, van Vugt M, Ezzet F. (1999) Clinical pharmacokinetics and pharmacodynamics of artemether- lumefantrine. Clinical Pharmacokinetics 37: 105-125. DOI: 10.2165/00003088-199937020-00002
Udomsangpetch, R., B. Pipitaporn, K. Silamut, R. Pinches, S. Kyes, S. Looareesuwan, C. Newbold, and N. J. White. (2002) Febrile temperatures induce cytoadherence of ring-stage Plasmodium falciparum-infected erythrocytes. Proceedings of the National Academy of Science of the United States of America 99:11825–11829. DOI: 10.1073/pnas.172398999
Achan J, Kakuru A, Ikilezi G, Ruel T, Clark TD, Nsanzabana C. (2012) Antiretroviral Agents and Prevention of Malaria in HIV-Infected Ugandan Children.
New England Journal of Medicine 367(22):2110±8. Epub 2012/11/30. DOI: 10.1056/NEJMoa1200501
Hobbs CV, Gabriel EE, Kamthunzi P, Tegha G, Tauzie J, Petzold E. (2016) Malaria in HIV-Infected Children Receiving HIV Protease-Inhibitor- Compared with Non-Nucleoside Reverse Transcriptase Inhibitor-Based Antiretroviral Therapy, IMPAACT P1068s, Sub-study to P1060. PLoS ONE 11(12): e0165140. DOI:10.1371/journal. pone.0165140
Oshikoya, K. A, Oreagba, I. A, Lawal, S., Awodele, O., Ogunleye, O. O., Senbanjo, I. O., Olayemi, S.O., Akanmu, S. A. (2014). Potential drug-drug interactions in HIV- infected children on antiretroviral therapy in Lagos, Nigeria. HIV/AIDS (Auckland, N.Z.) 6, 49–59. http://doi.org/10.2147/HIV.S52266
Khoo, S., D. Back, and P. Winstanley. (2005) The potential for interactions between antimalarial and antiretroviral drugs. AIDS 19:995–1005. DOI: 10.1097/01.aids.0000174445.40379.e0
Katrak S, Gasasira A, Arinaitwe E, Kakuru A, Wanzira H, Bigira V, Sandison TG, Homsy J, Tappero JW, Kamya MR, and Dorsey G. (2009) Safety and tolerability of artemether-lumefantrine versus dihydroartemisinin- piperaquine for malaria in young HIV-infected and uninfected children. Malarial Journal 8:272. DOI: 10.1186/1475-2875-8-272
Tavul L, Hetzel MW, Teliki A, Walsh D, Kiniboro B, Rare L, Pulford J, Siba PM, Karl S, Leo Makita L, Robinson L, Kattenberg JH, Laman M, Oswyn G, and Mueller I. (2018) Efficacy of artemether–lumefantrine and dihydroartemisinin–piperaquine for the treatment of uncomplicated malaria in Papua New Guinea. Malarial Journal 17:350. DOI: 10.1186/s12936-018-2494-z
Oguche S, Okafor HU, Watila I, Meremikwu M, Agomo P, Ogala W, Agomo C, Ntadom G, Banjo O, Okuboyejo T, Ogunrinde G, Odey F, Aina O, Sofola T, and Sowunmi A. (2014). Efficacy of Artemisinin-Based Combination Treatments of Uncomplicated Falciparum Malaria in Under-Five-Year-Old Nigerian Children. American Journal of Tropical Medicine and Hygiene 91(5), 925–935. DOI: 10.4269/ajtmh.13-0248
Kakuru A, Jagannathan P, Arinaitwe E, Wanzira H, Muhindo M, Bigira V, Osilo E, Homsy J, Kamya MR, Tappero JW, and Dorsey G. (2013) The Effects of ACT Treatment and TS Prophylaxis on Plasmodium falciparum Gametocytemia in a Cohort of Young Ugandan Children. American Journal of Tropical Medicine and Hygiene 88(4), 736–743. DOI: 10.4269/ajtmh.12-0654
World Medical Association Declaration of Helsinki: (2013) Ethical principles for medical research involving human subjects. The Journal of the American Medical Association 310 (20), 2191 – 4. http://doi.org/10.1001/jama.2013.281053.
Ashley EA, Stepniewska K, Lindegardh N, (2007) How much fat is necessary to optimize lumefantrine oral bioavailability? Tropical Medicine and International Health 12: 195 – 200. DOI: 10. 111/j. 1 3 6 5 -3156.2006.01784.x
O'Meara W. P., Barcus M, Wongsrichanalai C. (2006) Reader technique as a source of variability in determining malaria parasite density by microscopy,” Malaria Journal 5 article 118. DOI: 10.1186/1475-2875-5-118
Hammami I, Nuel G, and Garcia A, (2013) Statistical properties of parasite density estimators in Malaria. PLoS ONE, vol. 8, no. 3, Article ID e51987. DOI: 10.1371/journal.pone.0051987
WHO, (2010) Basic Malaria Microscopy, World Health Organization, Geneva, Switzerland, http://whqlibdoc.who.int/publications/2010/9789241547826_eng.pdf
Adu-Gyasi D, Adams M, Amoako S, (2012) Estimating malaria parasite density: assumed white blood cell count of 10,000/μl of blood is appropriate measure in Central Ghana,” Malaria Journal, vol. 11, article 238. DOI: 10.1186/1475-2875-11-238
Zlotkin S, Newton S, Aimone A.M. (2013) Effect of iron fortification on malaria incidence in infants and young children in Ghana: a randomized trial,” The Journal of the American Medical Association 310 (9) 938–947. DOI: 10.1001/jama.2013.277129
World Health Organization (2009) Methods for surveillance of antimalarial drug efficacy. Geneva. 9789241597531_eng.pdf;sequence=1 (who.int)
Maganda, B.A., Ngaimisi, E., Kamuhabwa, A. R., Aklillu, E. and Minzi. O. M. R. (2015) The influence of nevirapine and efavirenz-based anti-retroviral therapy on the pharmacokinetics of lumefantrine and anti-malarial dose recommendation in HIV-malaria co-treatment. Malarial Journal 14: 179-184. DOI: 10.1186/s12936-015-0695-2
World Health Organization (2015) WHO Guidelines for the treatment of malaria. 3rd ed . Geneva. https://apps.who.int/iris/handle/10665/162441 Accessed September 20, 2021
World Health Organization (2017) Artemisinin and artemisinin-based combination therapy resistance. In: Ringwald P, editor. Drug efficacy and response. Geneva. Available at https://apps.who.int/iris/bitstream/handle/10665/274362/
WHO-CDS-GMP-2018.18-eng.pdf. Accessed September 20, 2021
Ittarat W, Pickard AL, Rattanasinganchan P, Wilairatana P, Looareesuwan S, Emery K, Low J, Udomsangpetch R, Meshnick SR, (2003) Recrudescence in artesunate-treated patients with falciparum malaria is dependent on parasite burden not on parasite factors. American Journal of Tropical Medicine and Hygiene 68: 147–152.
Egunsola O and Oshikoya KA (2013) Comparative safety of artemether-lumefantrine and other artemisininbased combinations in children: a systematic review. Malarial Journal, 12:385. DOI: 10.1186/1475-2875-12-385
Bakshi R, Hermeling-Fritz I, Gathmann I, Alteri E. (2000) An integrated assessment of the clinical safety of artemether-lumefantrine: A new oral fixed-dose combination antimalarial drug. Transactions of The Royal Society of Tropical Medicine and Hygiene, 94:419-24. DOI: 10.1016/s0035-9203(00)90126-3
Parikh S, Kajubi R, Huang L, Ssebuliba J, Kiconco S, Gao Q, Li F, Were M, Kakuru A, Achan J, Mwebaza N, and Aweeka FT. (2016) Antiretroviral Choice for HIV Impacts Antimalarial Exposure and Treatment Outcomes in Ugandan Children. Clinical Infectious Diseases, 63(3):414-422. DOI: 10.1093/cid/ciw291
Nsanzabana C. and Rosenthal PJ. (2011) In Vitro Activity of Antiretroviral Drugs against Plasmodium falciparum. Antimicrobial Agents and Chemotherapy, 55 (11). DOI: 10.1128/AAC.05130-11
Azevedo R, Mendes AM, Prudêncio M. (2020) The Impact of Antiretroviral Therapy on Malaria Parasite Transmission. Frontiers in Microbiology, 24; 10:3048. DOI: 10.3389/fmicb.2019.03048
Views | PDF Downloads:
837
/ 310
/ 0
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.


