Pattern of drug utilisation, medication adherence, and treatment satisfaction among diabetic patients in a secondary hospital in southern Nigeria
Keywords:
Antidiabetic Drugs, Medication Adherence, Treatment SatisfactionAbstract
Background: Drug use evaluations provide insights into the effiffifficiency of drug use and may promote rational use of drugs, medication adherence and patient satisfaction with treatment. This study seeks to determine the current pattern of utilization of antidiabetic drugs, patient's adherence, and satisfaction with treatment among diabetic patients in a secondary hospital in southern Nigeria.
Methods: A cross sectional prospective antidiabetic drug utilization study was conducted among patients with diabetes mellitus receiving care at General Hospital, Ikot Ekpene between November 2019 and February 2020. Data on antidiabetic drug use pattern was obtained via an assessment of patients' prescriptions. Patients' medication adherence and satisfaction with treatment offffered was assessed using the 4-Item Morisky Medication-Taking Adherence Scale and the Treatment Satisfaction Questionnaire for Medication (Version 1.4). Descriptive statistics was used to summarize data, inferential statistics was used where applicable with statistical signifificance set at p<0.05.
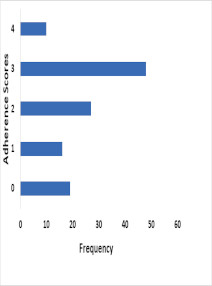
Results: The Sulphonylureas were the most frequently prescribed class of antidiabetic drugs (69.2%). A combination of antidiabetic agents was prescribed in 80.8% of the patients. Clinically signifificant and potentially dangerous drug-drug interactions was identifified in 91.7% of the prescriptions. The mean global satisfaction with treatment scores of the patients was 61.4(±8.3). The mean medication adherence scores of the patients was 2.1(±1.2). There was a statistically signifificant relationship between patients' global satisfaction with treatment score and the medication adherence score (r = 0.350; p = 0.0001).
Conclusion: Sulphonylureas were the most frequently used class of antidiabetic agents in this population. Patients were generally satisfified the treatment offffered. However, the level of adherence to prescribed antidiabetic drugs was poor. There is a compelling need for greater involvement of pharmacists in the provision of clinical services for patients with diabetes mellitus.
References
Indukar MS, Maurya AS, Indukar S (2016). Oral manifestations of diabetes. Clin Diabetes 2016 J an; 34 (1): 54 – 57 https://doi:10.2337/diaclin.34.1.54 Satpathy
SV, DattaS, Upreti B (2016). Utilization study of antidiabetic agents in a teaching hospital of Sikkim and adherence to current standard treatment guidelines. J Pharm Bioallied Sci. 2016 Jul-Sep; 8(3): 223–228. https://doi:10.4103/0975-7406.175975
Wettermark B, Hammar N, Michael FC, Leimanis A, Otterblad OP, Bergman U (2007). The new Swedish prescribed drug register opportunities for pharmacoepidemiological research and experience from the first six months. Pharmacoepidemiol Drug Saf. 2007; 16:726-35. https://doi:10.1002/pds.1294
Sachdeva PD, Pate BG (2010). Drug utilization studies – scope and future perspectives. International Journal of Pharmaceutical and biological research. Vol 1(1) 2010:11-17. Corpus ID: 20072257
Lam WY & Fresco P(2015). Medication adherence measures: An overview. BioMed Research International; 2015; 12. Article ID 217047. Hindawi Publishing Corporation. https://doi:10.1155/2015/217047
Khan A, Al-Abdul Lateef Z, Al Aithan M, Bu-Khamseen M, Al Ibrahim I, Khan S (2012). Factors contributing to noncompliance among diabetics attending primary health centers in the Al Hasa district
of Saudi Arabia. Journal of Family & Community Medicine; 2012 Jan;19(1):26-32. https://doi:10.4103/2230-8229.94008
Garc´ıa-P´erez LE, Alvarez M, Dilla T, Gil-Guill´en V, Orozco-Beltr´an D (2013). Adherence to therapies in patients with type 2 diabetes. Diabetes Therapy; 2013 Dec; 4(2): 175 - 94. https://doi:
1007/s13300-013-0034-y
Abebaw M, Messele A, Hailu M, Zewdu F (2016). Adherence and associated factors towards antidiabetic medication among Type II diabetic patients on follow-up at University of Gondar hospital, northwest Ethiopia. Advances in NursingVolume 2016, Article ID 8579157, 7 pages. https://dx.doi.org/10.1155/2016/8579157
Mann DM, Ponieman D, Leventhal H, Halm EA (2009). Predictors of adherence to diabetes medications: the role of disease and medication beliefs. Journal of Behavioral Medicine ; 2009 Jun;32(3):278-84. https://doi: 10.1007/s10865-009-9202-y
Omar MS & San KL (2014). “Diabetes knowledge and medication adherence among geriatric patient with type 2 diabetes mellitus. International Journal of Pharmacy and Pharmaceutical Sciences, vol. 6, Issue 3, pp. 103–106, 2014. ISSN- 0975-1491.
Yekta Z, Pourali R, Aghassi MR, Ashragh N, Ravanyar L, Pour MY (2011). Assessment of self-care practice and its associated factors among diabetic patients in urban area of Urmia, northwest of Iran. Journal of Research in Health Sciences; 2011 Jun 13;11(1):33-8. PMID: 22911945.
Kalyango JN, Owino E, Nambuya AP(2008). Non-adherence to diabetes treatment at mulago hospital in Uganda: prevalence and associated factors. African Health Sciences; 2008(2):67-73. PMID: 19357753.
Pascal IG, Ofoedu JN, Uchenna NP, Nkwa AA, Uchamma GU (2012). Blood glucose control and medication adherence among adult type 2 diabetic Nigerians attending a primary care clinic in under-resourced environment of eastern Nigeria. North American Journal of Medical Sciences; 2012 Jul; 4(7): 310 - 5. https//doi:10.4103/1947-2714.98590.
Vermersch P, Hobart J, Dive-Pouletty C, Bozzi S, Hass S, Coyle PK (2017). Measuring treatment satisfaction in MS: Is the treatment satisfaction questionnaire for medication fit for purpose? Multiple Sclerosis Journal 2017, Vol. 23(4) 604–613. https://doi: 10.1177/ 1352458516657441
Pascal IG, & Nkwa AA (2016). Diabetes treatment satisfaction, medication adherence, and glycemic control among ambulatory type 2 diabetic Nigerians in a primary care clinic of a tertiary hospital situated in a resourcelimited environment of southeast Nigeria. Archives of Medicine and Health Sciences; 2016, Vol. 4, Issue 3, page 169-174. https://doi:10.4103/2321-4848.196215
Israel GD (2013). Determining sample size. Publication of the Agricultural Education and communication department, Florida cooperative extension service, Institute of food and agricultural sciences, University of Florida; June, 2013.
Gerardo S (2018). The Morisky medication adherence scale: an overview. 2018.https://www.pillsy.com/articles/the- morisky-medication-adherence-scale- definition-alternatives-and-overview Accessed on May 02, 2020
Sjoqvist F. & Birkett D (2003). Drug Utilization. In Bramle y D.W.Ed. Introduction to drug utilization research. WHO booklet. New York: WHO office of publication; 2003. pp. 76-84.
Lau GS, Chan JC, Chu PL, Tse DC, Critchely JA (1996). Use of antidiabetic and antihypertensive drugs in hospital and outpatient settings in Hong Kong. Ann Pharmacother. 1996; 30:232–7. https://doi:
1177/106002809603000304.
Xavier D, Nagarani MA, Srishyla MV (1999). Drug utilization study of antihypertensives and antidiabetics in an Indian referral hospital. Indian J Pharmacol. 1999;31:241–2.
Al Khaja KA, Sequeira RP, Mathur VS (2001). Prescribing patterns and therapeutic implications for diabetic hypertension in Bahrain. Ann Pharmacother. 2001; 35: 1350 – 9. https://doi.org/10.1345/aph.10399
Sutharson L, Hariharan RS, Vamsadhara C (2003). Drug utilization study in diabetology outpatient setting of a tertiary hospital. Indian J Pharmacol. 2003;35(4):237–2.
Agarwal AA, Jadhav PR, Deshmukh YA (2014). Prescribing pattern and efficacy of anti-diabetic drugs in maintaining optimal glycemic levels in diabetic patients. J Basic Clin Pharm. 2014; 5: 79 – 83. https://doi:10.4103/0976-0105.139731
Upadhyay DK, Palaian S, Ravi Shankar P, Mishra P, Sah AK (2007). Prescribing pattern in diabetic outpatients in a tertiary care teaching hospital in Nepal. J Cardiovasc Dis Res. 2007;4:248–55.
Das P, Das BP, Rauniar GP, Roy RK, Sharma SK (2011). Drug utilization pattern and effectiveness analysis in diabetes mellitus at a tertiary care centre in eastern Nepal. Indian J Physiol Pharmacol. 2011;55:272–80. PMID: 22471235.
Johnson JA, Pohar SL, Secnik K, Yurgin N, Hirji Z (2006). Utilization of diabetes medication and cost of testing supplies in Saskatchewan. BMC Health Serv Res.2006 Dec., 6:159. https://doi:10.1186/1472-6963-6-159
Nathan DM, Buse JB, Davidson MB, Ferrannini E, Holman RR, Sherwin R, & Zinman B (2009). Medical management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy: A consensus statement from the American Diabetes Association and the European Association for the study of diabetes. Diabetes Care. 2009; 32(1):193–203. https://doi.org/10.2337/dc08-9025
Hermann LS, Scherstén B, Bitzén PO, Kjellström T, Lindgärde F, Melander A. (1994). Therapeutic comparison of metformin and sulfonylurea, alone and in various combinations. A double-blind controlled study. Diabetes Care 1994 17(10): 1100 - 1109. https://doi.org/10.2337/diacare.17.10.1100
Fernandez O, Duran E, Ayuso T, Hernandez L, Bonaventura I, Forner M (on behalf of the STICK Study Investigators Group) (2017). Treatment Satisfaction with Injectable Disease-Modifying Therapies in
Patients with Relapsing-remitting Multiple Sclerosis. (the STICK study). PLoS ONE. 2017; 12(10): e0185766 . https://doi.org/10.1371/journal.pone.0185766.
Turner AP, Kivlahan DR, Sloan AP, Haselkorn JK (2007). Predicting ongoing adherence to disease modifying therapies in multiple sclerosis: utility of the health beliefs model. Mult Scler Houndmills Basingstoke Engl. 2007; 13: 1146 ± 1152. 2007 Nov; 13 (9): 1146 - 5 2. https://doi:10.1177/1352458507078911
Steinberg SC, Faris RJ, Chang CF, Chan A, Tankersley MA (2010). Impact of adherence to interferons in the treatment of multiple sclerosis: a non-experimental, retrospective, cohort study. Clin Drug Investig. 2010;30(2):89-100. https://doi: 10.2165/11533330-000000000-00000
Ibinda F, Mbuba CK, Kariuki SM, Chengo E, Ngugi AK, Odhiambo R, Lowe B, Fegan G, Carter JA, Newton CR (2014). Evaluation of Kilifi epilepsy education programme: A randomized controlled trial.
Epilepsia. 2014: 55(2): 344 - 52. https://doi:10.1111/epi.12498
Jeannie KL, Karen AG, Allen JT (2006). Effect of a pharmacy care program on medication adherence and persistence, blood pressure and low-density lipoprotein cholesterol. A randomized controlled trial.
JAMA. 2006 Dec 6;296(21):2563-71. https://doi: 10.1001/jama.296.21.joc60162
Eshiet U, Okonta J, Ukwe C (2018). Pharmaceutical Care Intervention Improves Adherence to Antiepileptic Medication. Journal of Pharmaceutical Research International. 23(6): 1-11, 2018; Article no.
JPRI. 44377 https://doi:10.9734/JPRI/2018/44377.
Hepler CD & Strand LM (1990). Opportunities and responsibilities in pharmaceutical care. American Journal of Health Systems Pharmacy. 1990; 47:533-543. PMID: 2316538.
American Society of Health-System Pharmacists (1996). ASHP guidelines on a standardized method for pharmaceutical care. AmJ Health -Syst Pharm. 1996: 15; 53 ( 1 4 ) : 1 7 1 3 - 6 . h tt p s :// d o i:
1093/ajhp/53.14.1713
Atkinson MJ, Kumar R, Cappelleri JC, & Hass SL (2005). Hierarchical construct validity of the treatment satisfaction questionnaire for medication (TSQM version II) among outpatient pharmacy consumers. Value Health 2005; 8(Suppl. 1): S9–S24. https://:10.1111/j.1524-4733.2005.00066.x
Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D (2012). A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence 2012; 6:39-48. https://doi:10.2147/PPA.S2475239. Nicolucci A, Cucinotta D, Squatrito S, Lapolla A, Musacchio N, Leotta S, Vitali L,
Bulotta A, Nicoziani P, Coronel G (on behalf of QuoLITy study Group) (2009). Clinical and socio-economic correlates of quality of life and treatment satisfaction in patients with type 2 diabetes. Nutr Metab Cardiovasc Dis. 2009 Jan; 19(1) 45 - 53. https://doi:10.1016/j.numecd.2007.12.005
Turner RR, Testa MA, Hayes JF, Su M (2013). Validation of the allergic rhinitis treatment satisfaction and preference scale. Allergy Asthma Poc. Nov - Dec 2013; 34 (6) : 551 - 7 . https://doi:
2500/aap.2013.34.3715
Haase R, Kullmann JS, Ziemssen T (2016). Therapy satisfaction and adherence in patients with relapsing remitting multiple sclerosis: the THEPA-MS survey. Ther Adv Neurol Disord. 2016 Jul;9(4):250-63. https://doi: 10.1177/1756285616634247
Klauer T & Ze ttl U K (2008). Compliance, adherence, and the treatment of multiple sclerosis. J Neurol. 2008: 255 Suppl 6:87-92. https://doi: 10.1007/s00415-008-6016-8
Views | PDF Downloads:
1145
/ 357
/ 0
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.