Modulating inflammation in COVID-19 viral disease: The emerging role for dexamethasone
Keywords:
Covid-19 virus disease, Inflammation, DexamethasoneAbstract
Background: The global scientific community continues to saddle one of the responsibilities of constraining the menace caused by Coronavirus Disease 2019 (COVID-19); a relatively novel corona virus infection that has metamorphosed to becoming a pandemic. Epidemiological evidence shows that it is responsible for over 1.7 million death worldwide. Besides, the pandemic has negatively impacted vital sectors of national economy and government such as employment of labor, transportation, national budgets and financial business progression. Conversely, the times have driven scientists, medical experts and health professionals to thinking up newer and safer therapeutic strategies in order to better manage and combat the virus. While several therapeutic approaches have been unveiled by researchers, this article lays emphasis on modulating inflammation in COVID-19 viral disease with respect to an emerging role for dexamethasone. Crosstalk between pathogenesis of Severe Acute Respiratory Syndrome-related Coronavirus-2 (SARSr-CoV-2) and inflammation remains invaluable to unraveling other alternative drug targets that may pose as probable paths towards mitigating the effects of the virus in humans.
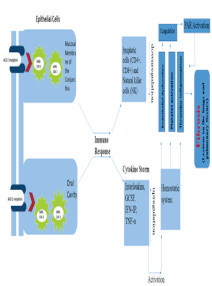
Methods: The roles of angiotensin converting enzyme-2 protein in mediating the transfer of SARSr-CoV-2 into epithelial cells of the mucosal membranes of the conjunctiva and oral cavity was evaluated. Also, viral antigen presentation in the cells was evaluated as a trigger to an immunological reaction that results in a cytokine surge in the blood, downplay of lymphocytic cells and upregulation of other chemical mediators of inflammation. This eventually actuates the hemostatic system to trigger pro coagulating factors and thrombo-inflammatory responses, which may ultimately lead to fibrosis and other respiratory disorders.
Conclusion: The ameliorative effect of dexamethasone, a commonly used glucocorticoid for treating inflammatory disorders remains striking and significant in SARSr-CoV-2 management. Contrary to data gotten from previous studies of glucocorticoids effect on earlier existing corona viruses, recent findings have reported that dexamethasone possess some beneficial effects in attenuating pulmonary derangements caused by SARSr-CoV-2. Moreover, this brings to limelight and further buttresses the relationship between inflammation and COVID-19 pathology. Hence, the need to discover newer or repurpose preexisting drug molecules that may target inflammatory signaling cascades in COVID-19mviral disease is imperative.
References
Fan Y, Zhao K, Shi ZL, Zhou P(March 2019). "Bat Coronaviruses in China". Viruses. 11 (3): 210.
Cherry J, Demmler-Harrison G, Kaplan S, Steinbach W, Hotez P(2017). Feigin and Cherry's Textbook of Pediatric Infectious Diseases. Elsevier Health Sciences. https://www.elsevier.com/books/feigin-and- cherrys-textbook-of-pediatric-infectious-diseases/cherry/978-0-323-37692-1
Hui David, Azhar Esam, Madani Tariq, Ntoumi Francine, Kock Richard, Dar Osman, Ippolito Giuseppe, Mchugh Timothy, Memish Ziad, Drosten Christian, Zumla Alimuddin, Petersen Eskild (2020). –"The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health The latest 2019 novel coronavirus outbreak in Wuhan, China". International Journal of Infectious Diseases. (91): 264–266
David S. Hui and Alimuddin Zumla (2019). Severe Acute Respiratory Syndrome: Historical, Epidemiologic, and Clinical Features. Infectious Disease Clinics of North America. 33(4): 869-889.
U.S. Department of Labour. COVID-19 impact in Employment and Training Administration Washington DC (2020). https://www.dol.gov/coronavirus#Unemployment —"A third of the global population is on coronavirus lockdown here's our constantly updated list of countries and restrictions"
(2020). Business Insider. https://www.businessinsider.in/international/news/a-third-of-the-global-population-is-on- coronavirus-lockdown-x2014-hereaposs-our- constantly-updated-list-of-countries-and-restrictions/slidelist/75208623.cms
Le Tung T, Andreadakis Z, Kumar A, Román RG, Tollefsen S, Saville M (2020). The COVID-19 vaccine development landscape. Nature Reviews Drug Discovery. (19):305–6.
Novel Corona Virus 2019 Situation Updates WHO(2021).
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
Lau H, Khosrawipour V, Kocbach P, Mikolajczyk A, Ichii H, Schubert J, (2020). Internationally Lost COVID-19 Cases. Journal of Microbiology, Immunology, and Infection. 53 (3): 454–458.
Cui J, Li F, Shi ZL (2019). "Origin and evolution of pathogenic coronaviruses". Nature Reviews Microbiology. 17 (3): 181–92.
Rothan H., Byr a r eddy S. (2020). The epidemiology and pathogenesis of coronavirus disease outbreak. Journal of Autoimmunity. 109: 102433. https://doi.org/10.1016/j.jaut.2020.102433
Lalchhandama K (2020). "The chronicles of coronaviruses: the bronchitis, the hepatitis and the common cold". Science Vision. 20 (1): 43–53.
Letko, M., Munster, V., (2020). Functional assessment of cell entry and receptor usage for lineage B β-coronaviruses, including 2019-nCoV. BioRxiv. https://doi.org/10.1101/2020.01.22.915660.
Wan, Y., Shang, J., Graham, R., Baric, R.S., Li, F (2020). Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade - long structural studies of SARS coronavirus. Journal of Virology. https://doi.org/10.1128/JVI. 00127 - 20
Eckert, D.M., Kim, P.S., (2001). Mechanisms of viral membrane fusion and its inhibition. Annual Review of Biochemistry. 70, 777–810. https://doi.org/10.1146/annurev. biochem.70.1.777
Hu J, Jolkkonen J, Zhao C. (2020). Neurotropism of SARS-CoV-2 and its neuropathological alterations: Similarities with other coronaviruses. Neuroscience and Biobehavioral Reviews. (119) 184–193.
Chen, T., Wu, D., Chen, H., Yan, W., Yang, D., Chen, G., Ma, K., Xu, D., Yu, H., Wang, H., Wang, T., Guo, W., Chen, J., Ding, C., Zhang, X., Huang, J. , Han, M., Li, S, Luo X . ,Zhao, J., Ning, Q., (2020) Clinical characteristics of 13 deceased patients with coronavirus disease 2019: retrospective study. BMJ. https:// doi.org/10.1136/bmj.m1091.
S.A. Azer (2020). COVID-19: pathophysiology, diagnosis, complications and investigational therapeutics. New Microbes and New Infections. 37: 100738. https://doi.org/10.1016/j.nmni.2020.100738
Zahid A, Li B, Kombe A.J.K., Jin T, Tao J (2019). Pharmacological Inhibitors of the NLRP3 Inflammasome. Frontiers in Immunology. 10: 2538
Di Raimondo D, Tuttolomondo A, Buttà C, Miceli S, Licata G, Pinto A. (2012). Effects of ACEinhibitors and angiotensin receptor blockers on inflammation. Current Pharmaceutical Design. 18(28):4385-413.
Huang Q, Wu X, Zheng X, Luo S, Xu S, Weng J. (2020) Targeting inflammation and cytokine storm in COVID-19. Pharmacological Research. 159:105051.
Md Insiat Islam Rabby (2020). Current Drugs with Potential for Treatment of COVID-19: A Literature Review. Journal of Pharmacy and Pharmaceutical Sciences. 23 (1):58-64.
Horby P, Wei Shen Lim , Jonathan R Emberson , Marion Mafham , Jennifer LBell , Louise Linsell , Natalie Staplin , Christopher Brightling , Andrew Ustianowski , Einas Elmahi , Benjamin Prudon (2021). Dexamethasone in hospitalized patients with covid-19 preliminary report. New England Journal of Medicine. 384 (8):693-704.
“Dexamethasone” (2017). The American Society of Health - System Pharmacists. https://web.archive.org/web/20170831175940/https://www.drugs.com/monograph/dexamethasone.html
Roderick Flower, Felicity Gavins (2008). xPharm: The Comprehensive Pharmacology Reference. https://www.sciencedirect.com/topics/nursing-and-health-professions/pregnanederivative
Toth G., Kloosterman C., Uges R., Jonkman F. (1999). Pharmacokinetics of High-dose Oral and Intravenous Dexamethasone. Therapeutic Drug Monitoring. 21(5): 532.
Medicine Net Dexamethasone: https://www.medicinenet.com/dexamethasone- d e c a d r o n - dexpak/article.htm#what_is_dexamethasone_and_how_does_it_work_mechanism_of_action
Mark G. Papich (2016). Saunders Handbook of Veterinary Drugs (Fourth Edition).
https://www.elsevier.com/books/saundershandbook-of-veterinary-drugs/9780323244855
Mukhtar H. Ahmed and Arez Hassan (2020). Dexamethasone for the Treatment of Coronavirus Disease (COVID-19): a Review. 2: 2637–2646.30. Marmor Meghan and Andrea Jonas (2020). “Corticosteroids for COVID-19-Associated ARDS.” Clinical Pulmonary Medicine. 27(6):165–167.
Downloads
Views | PDF Downloads:
414
/ 194
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.


